Introduction
Reshaping care pathways and healthcare systems around patients’ needs requires a standardized database on patient-centered outcomes. Standard sets as proposed by ICHOM serve as a basis for developing datasets that allow for comparisons across different patient populations thus drawing meaningful conclusions for enhancing quality of care. However, standardization of outcomes and statistical analyses require a common medical history set based on case-mix variables capturing demographic details, information on health status, lifestyle and social factors. These case-mix variables are a fixed component of every ICHOM set, nevertheless they vary in terms of domain name and corresponding question across sets.
As the largest provider of software for patient-centered outcomes in German speaking countries, Heartbeat Medical accumulated profound expertise in implementing ICHOM sets. To support the interoperable collection of standardized high quality data allowing for adequate benchmarking, a core medical history set based on the most commonly used case-mix variables in adult ICHOM sets is proposed.
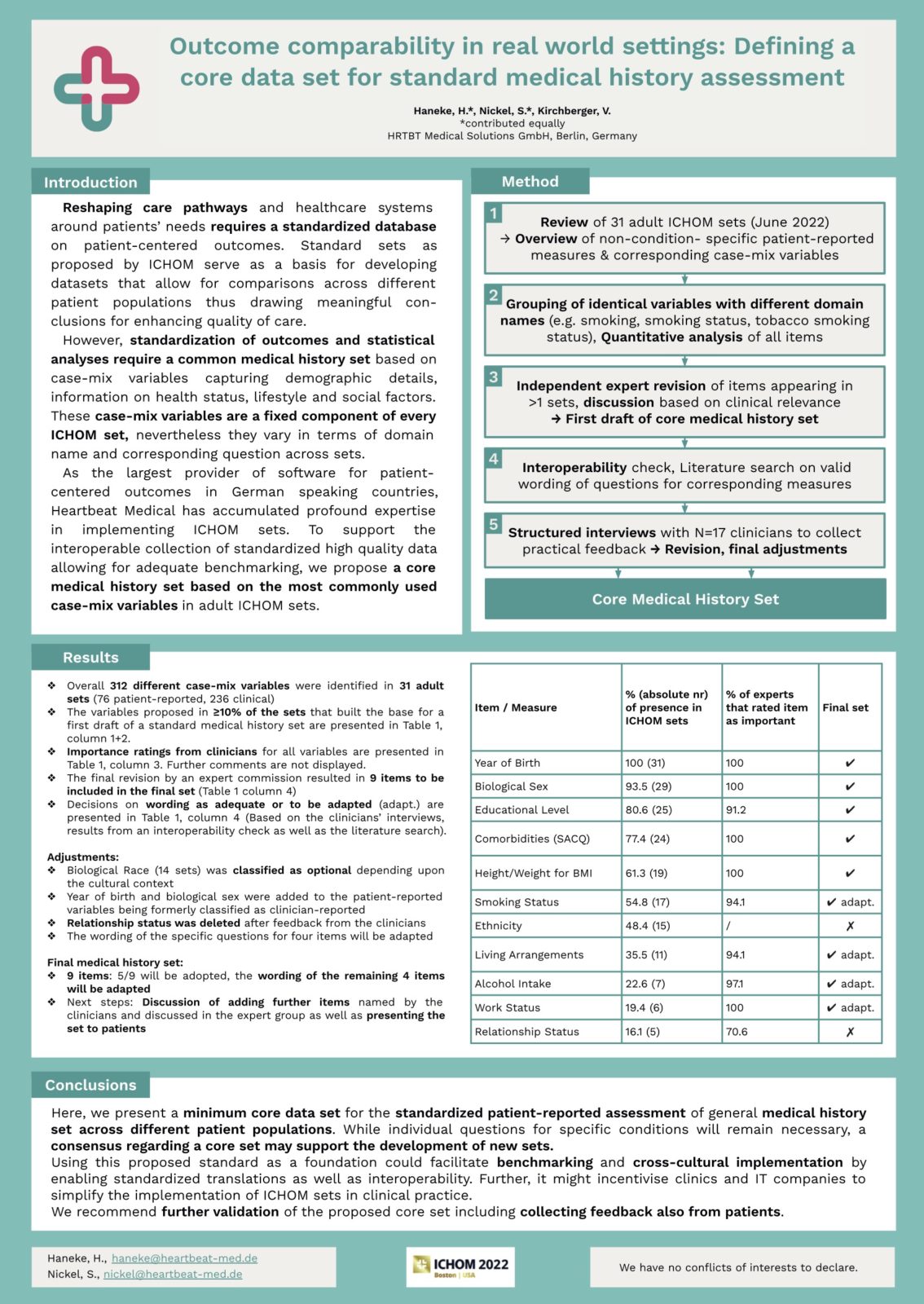
Methods
All 41 reference guides for ICHOM-sets were extracted from ICHOM Connect between May and June 2022. Pediatric sets were excluded for reasons of comparability. An overview of non-condition-specific patient-reported measures and corresponding case-mix variables was created. In some cases the same underlying variables are assigned different domain names (e.g. smoking, smoking status, tobacco smoking status), so these variables were grouped to adjust the specific wording for comparability assurance across sets.
A quantitative analysis of the items was conducted, including a ranking according to frequency of appearance. The most frequent domains and questions were then compiled and listed. In a second step, all items appearing in more than one set were independently revised by two experts and discussed based on clinical relevance, resulting in final adjustments. A check for interoperability was carried out. Last, interviews with clinicians were conducted to provide practical feedback on the relevance of the variables.
Results
Overall, a total number of 312 different case-mix variables were identified in 31 adult sets (76 patient-reported, 236 clinical). A standard medical history was drafted based on the most frequently recommended patient-reported variables proposed in more than 10% of the sets (percentage of sets question was covered in [total number]). These include year of birth (100 [31]), biological sex (93.5 [29]), educational level (80.6 [25]) using the International Standard Classification for Education ISCED, comorbidities (77.4 [24]) assessed by the Self-Reported Comorbidity Questionnaire (SACQ), height and weight for BMI calculation (61.3 [19]), smoking status (54.8 [17]), ethnicity (48.4 [15]), living arrangements (35.5 [11]), alcohol intake (22.6 [7], summarized different question types), work status (19.4 [6]), relationship status (16.1[5]). Adjustments in the second step included for instance biological race (14) being classified as optional depending upon the cultural context. Year of birth and biological sex were added to the patient-reported variables being formerly classified as clinician-reported. A core data set consisting of 12 patient-reported case-mix variables with a consistent wording was created.
Conclusions
The study at hand presents a minimum core data set for the standardized patient-reported assessment of general medical history set across different patient populations. While individual questions for specific conditions will remain necessary, a consensus regarding a core set may support the development of new sets.
By using this proposed standard as a foundation, benchmarking and cross-cultural implementation by enabling standardized translations as well as interoperability could be facilitated. Further, it might incentivise clinics and IT companies to simplify the implementation of ICHOM sets in clinical practice. We recommend further validation of the proposed core set including collecting feedback also from patients.